How can we help?
888-283-1722
Call us now at 888-283-1722
24/7 Referrals and Nursing Support
In the News
North Shore Medical Partnership Seeks Earlier End-Of-Life Conversations
May 30, 2018WBUR
During a routine primary care checkup, Dr. Rebecca Lee opens a difficult conversation with Stacey Regal-O’Hare, who has a serious illness: "What are your goals for the end of life?" (Martha Bebinger/WBUR)
It starts off like a regular medical checkup at a physician's office in Danvers. Then Dr. Rebecca Lee pauses for a minute and holds her patient’s gaze."Today, Stacey, I want to ... kind of hit the pause button and see where you’re at," Lee says, "what you are thinking about your illness and what your goals are."
Goals for the last stage of life. Stacey Regal-O’Hare isn’t there, but she does have a serious illness, and Lee, of North Shore Physicians Group, wants to document her patient’s preferences before there’s a crisis moment in an emergency room or ICU.
"I like to do that when folks are actually feeling well. Do you feel comfortable with that?" asks Lee. "Yeah," replies Regal-O'Hare, softly.
Such conversations with a primary care doctor are rare, and only 27 percent of Massachusetts patients with a serious illness have discussed their wishes with any physician, including a specialist. Earlier planning for the end of life is one element of a $750,000 grant-funded partnership between the North Shore Physicians Group and Care Dimensions, a nonprofit that offers hospice and palliative care.
Regal-O’Hare, 52, inherited a rare disease called von Hippel-Lindau syndrome that produces tumors, mostly benign.
"It can be dormant or it can be on fire, and right now I’m kind of in between," Regal-O'Hare tells Lee in response to a question about the state of her disease. She is having trouble with some daily activities.
"I need help with a lot of..." Regal-O'Hare pauses, choking on the words, "a lot of physical stuff. I can’t really cook any more 'cause I keep burning myself." Regal-O’Hare has lost feeling in her hands. One finger slipped into a pan recently while she was scrambling eggs but she didn't notice until she saw a blister rise on her skin.
"You’re amazing," says Lee, offering a tissue.
Dr. Lee glances down at questions on a cue card she received during a recent training for primary care physicians about how to have these difficult conversations with patients. Partners HealthCare, which includes the North Shore Physicians Group, expects to train all affiliated primary care doctors by 2020.
"If your health situation were to get worse," Lee asks, "what are your goals, what would be your wishes around that?"
"I would not want to be non-function -- I don’t even know how to express it -- like I don’t want to be on a vent and just here," Regal-O’Hare tells her doctor.
That's vent as in ventilator, if Regal-O’Hare becomes unable to breathe on her own.
The conversation continues for another 20 minutes. Lee and Regal-O’Hare discuss other life supports and health care proxies. Lee makes notes that anyone who checks the electronic medical record will see. They complete and both sign a bright pink sheet of paper commonly know as a MOLST, or Massachusetts Medical Order for Life-Sustaining Treatment. Regal-O'Hare will post it on her fridge, where EMTs responding to 911 calls are trained to look.
There's one last item on Lee's agenda for the visit. Through this program with Care Dimensions, Lee can refer Regal-O’Hare for palliative care, which might include pain management, nutrition counseling and help managing emotional stress at home.
"If you aren't ready, not interested today, we can revisit that down the line," Lee says, cautiously.
"I think with further investigation," Regal-O'Hare says, with a nervous laugh, "I would yeah, yes."
Fewer ER Visits, Lower Costs
That "yes" means Regal-O’Hare will get a call soon from Eileen Fagan, a nurse practitioner to discuss what additional support Regal-O’Hare needs, such as handicapped parking, more care at home or someone to help with grocery delivery.
"It’s about restoring the freedom to be comfortable, not think about your illness, and carry on," Fagan says.
Patients who have heart or breathing problems are asked to log vital signs daily on a tablet-style device. A nurse reviews the numbers, looking for early warnings like weight increases, fluid buildup and difficulty breathing.
A nurse "putting that all together can make a call to the primary care and maybe adjust [the patient's] medications before it gets too late and they would need an emergency department visit," says Susan Lysaght Hurley, program director for the project, known as Palliative Care+.
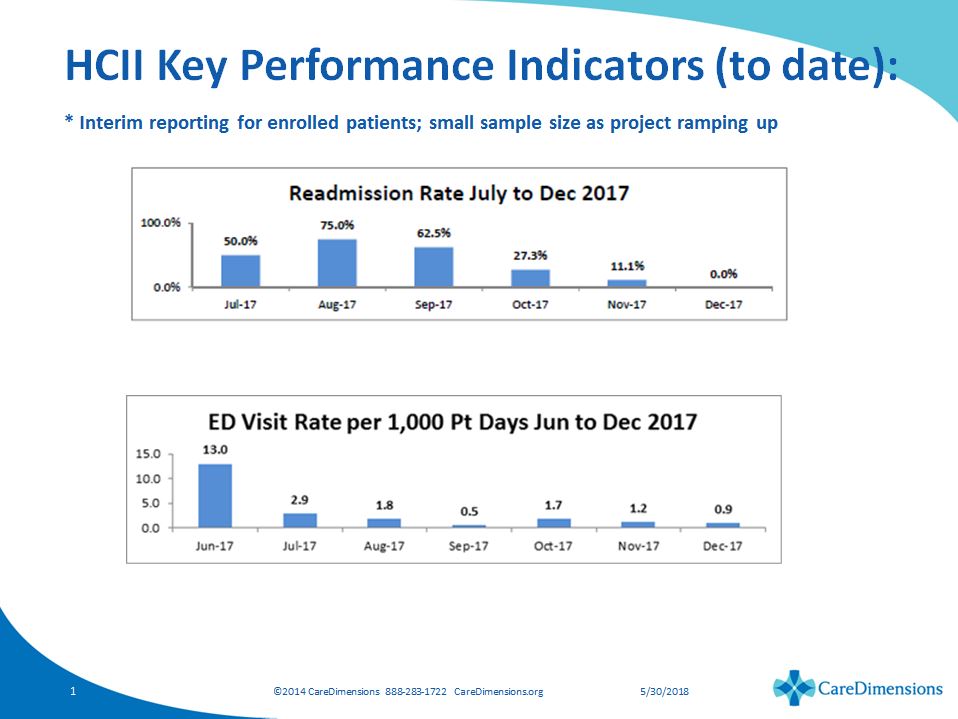
And that's how the project expects to save money. Emergency room visits and readmissions after hospitalizations are both down, based on the first few months of data. With those two changes, the $750,000 project grant from the state’s Health Policy Commission (HPC) is expected to save $7.2 million over the project's duration.
A nearly tenfold return on investment would have big implications. About 25 percent of Medicare dollars are spent during the last year of patients’ lives.
"So if we are looking for opportunities to control to health care costs, we see this opportunity at the end of life," says Sree Chaguturu, Partners' chief population health officer.
The Palliative Care+ project falls under the Partners Medicare Accountable Care Organization (ACO) and builds on two other end of life studies conducted by Partners physicians. It's unfolding amid some debate about whether hospice costs more than it saves and whether end-of-life expenses and the intensity of services patients are receiving are up or down. The project has not determined if enrolled patients are spending less than those who don't receive more assistance in the home and other supports.
But HPC members say they are impressed with the Palliative Care+ results.
"The promise here is that if we actually do what matters to people, if we focus on the needs of individuals, their lives and their deaths are more under their control," says Dr. Don Berwick, "and costs fall."
But Berwick points out a problem: The insurer gets the savings. There's no mechanism for North Shore doctors and nurses to use the money patients didn't spend on unnecessary ER visits or hospitalizations to sustain the project beyond its end date in November.
"So we’re going to have to think hard about the American health care payment system to allow programs like this to really thrive," says Berwick, who is also president emeritus and senior fellow at the Institute for Health Care Improvement.
There's no way to recoup savings, even in this case, in which patients are part of a shared savings payment model, the Medicare ACO.
As Chaguturu explains, the payers -- Medicare in this case -- don't look at whether individual programs within an ACO save money; the entire organizer has to clear a savings threshold before the providers can claim a share.
"You could be saving money in this program but other things are happening that prevent you from hitting your shared savings goal," says Chaguturu, "so the provider has no money to reinvest."
HPC director David Seltz says sustainability is a "huge challenge" for many of the 20 projects funded so far through the commission's Health Care Innovation Investment Program. But Seltz says other ACOs will "dramatically change the way health care will be paid for, so we think that this program is at the perfect time between the old health care system and the new health care system."
Any talk about saving money by spending less on patients as they approach death triggers fear among some families. Supporters of the Palliative Care+ program say patients who want intensive care right up to the end of life will get it.
"This is all about giving you control over your life, not taking things away from you," Berwick says.
This segment aired on May 30, 2018
Anyone—patient, family, care provider—can make a referral. Fill in the form online or call us today.
Since 1978, Care Dimensions, formerly Hospice of the North Shore, has provided comprehensive and compassionate care for individuals and families dealing with life-threatening illnesses. As the non-profit leader in advanced illness care, we offer services in over 100 communities in Massachusetts.
Copyright 2024 | Care Dimensions, 75 Sylvan Street, Suite B-102, Danvers, MA 01923 | 888-283-1722 | 978-774-7566 |